Inclusive health behaviour change

I am working to create a paradigm of behaviour change that works for fat, disabled people.
So much of popularised behaviour change is focused on weight loss or improving your body. But what if you just want to survive and thrive in your body, regardless of what it looks like?
For me, this is a personal journey
I am a behavioural scientist, with a PhD in health psychology (the psychology of physical health and illness). I’m a specialist in helping people to build products designed to change people’s health behaviours.
However, I’m also human. When I was young I was naturally slim, but as I got older, my weight gradually crept up. I spent years cycling between phases of punishing diets and exercising regimes, and “rebelling” by gaining back all the weight and more. In 2018 I was also diagnosed with a disability: hypermobility spectrum disorder. The best way to manage it is through physiotherapy-type exercises. However, my relationship with exercise had always been about weight loss, and had always been a phase of either doing “too much” or nothing at all. I really struggled with getting into a regular practice of the right kind of exercise, and my body suffered for it.
I’m supposedly an “expert” in helping people to do all the right things for their health, but I really struggle with sticking to it for myself.
Then, a couple of things changed for me.
Turning points
In 2018, I quit dieting. I discovered a world of influencers, writers, podcasters, and providers who were talking about accepting your fat body, and how a focus on body weight is unhelpful. There is evidence to back up this view, for example:
- The relationship between BMI and health outcomes isn’t linear (i.e. it isn’t always worse for your health to be fatter) - and even “obese” groups with a BMI of 30-35 have similar health outcomes to people in the “normal” range
- People can be fat and healthy, and slim and unhealthy
- “Weight cycling” (as I was experiencing) has been shown to be bad for your health
- Fundamentally, even if the above wasn’t true, it doesn’t matter because for most people, diets don’t work in the long-term. While people may see initial improvements, these effects tend to disappear a few months later.
This paper gives a great overview of the evidence - but I’ll also be sharing more on this in the future!
This inspired me to abandon the quest to be smaller, and instead work on accepting myself. I explored practices like intuitive eating and joyful movement. I gained weight, but it’s stabilised - I now identify as “fat” (I see it as a descriptor, rather than a negative thing). I’m much happier, but there’s still always a little niggle in my mind about my long-term health.
While this improved my relationship with food, exercise was still a struggle. I tried following the mantra of intuitive & joyful movement (i.e. moving in ways that you love - for me it’s dancing to Fitness Marshall routines 💃🏻), but I knew that there was a whole category of repetitive strength training exercises I needed to do for my body, that I didn’t find joyful, and so found it hard to stick to.
Then in 2024, I discovered a very specialist exercise programme (from the brilliant Chimera Health), designed for people like me. For the first time, I found myself sticking to it - exercising multiple days a week, in a way that suited my bendy body, and progressing over time. Eight months later, and I’m still going. I feel for the first time like I’m caring for my body, not seeking to change or punish it - and it makes me feel good.
In both cases, what unlocked me was experts in a different paradigm of approaching food and exercise, to those which I’d seen in my health psychology training, and in mainstream behaviour change support (oh, the years I gave to My Fitness Pal and Strava that I’ll never get back!). I did use some of my behavioural science learnings (particularly when trying to form new habits), but generally it felt like the journey I was on with my own body was disconnected from the behavioural science that I was doing at work. I recall working on a project involving Type 2 Diabetes, and hearing harrowing stories of patients who were blaming themselves, or avoiding seeking healthcare for worrying symptoms because “the doctor will just tell me to lose weight”. I wanted to scream “there must be another way for you!”, but I felt ill-equipped to apply a fat-accepting, disability-inclusive behavioural science - when most of the world was still focussed on making bodies smaller and more “perfect”.
Weight-neutral, disability-inclusive health behaviour change
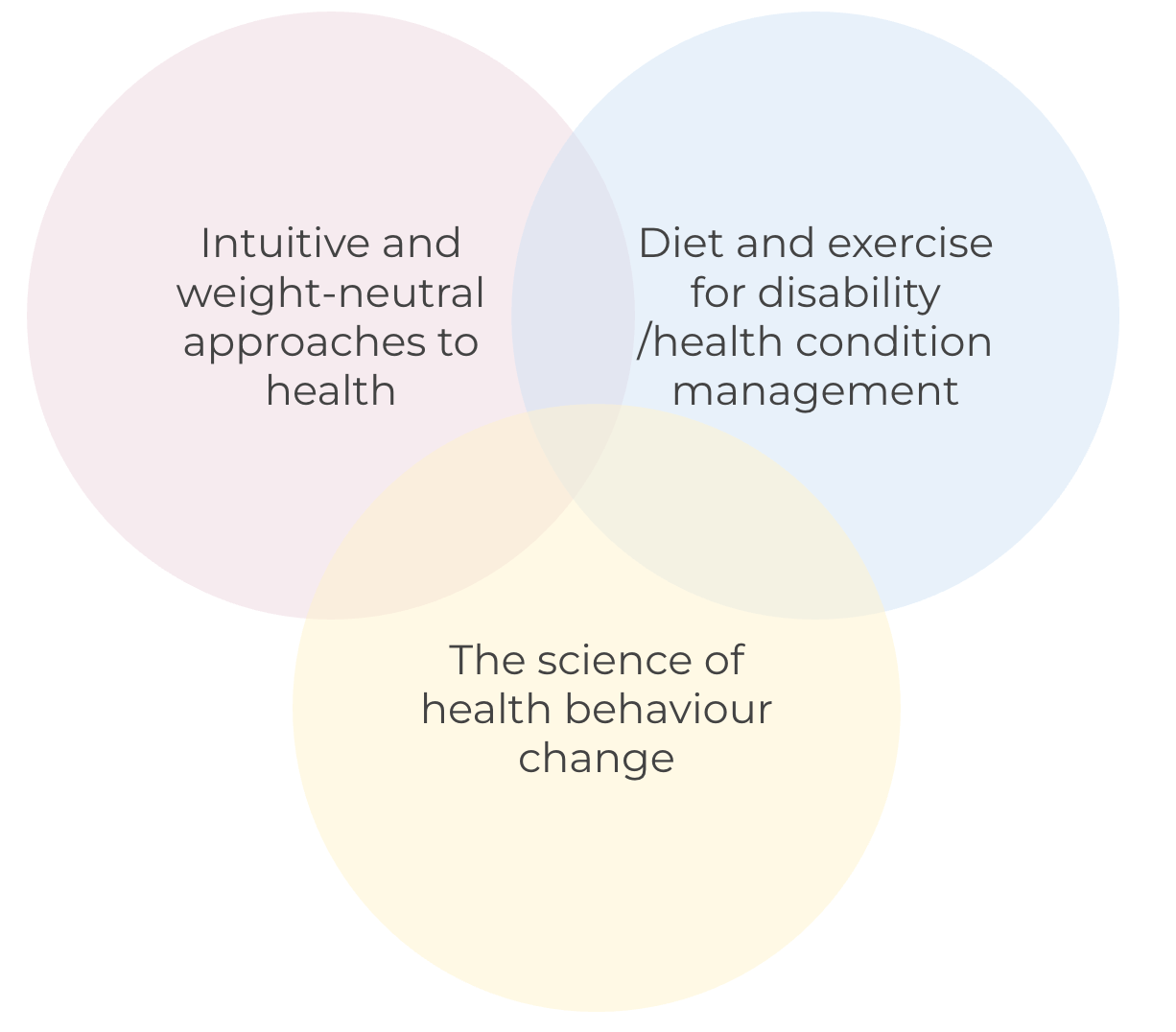
I believe that there’s so much good and useful stuff out there in the realms of weight-neutral and intuitive approaches to diet and exercise, tailored exercise support for people with disabilities, and the science of changing behaviour. The space I play in is at the intersection of these things, to explore what a fully inclusive approach to health behaviour change looks like, for fat and/or disabled people like me. How can we improve our health, while still feeling happy in, and accepting of, our bodies? How can we move and eat in an intuitive way, when our bodies need specific things? How does behavioural science need to change and adapt in order to support this approach?
There is research into what exercise behaviour change looks like for people with chronic health conditions and disabilities - largely it suggests that programmes should be tailored to the individuals’ condition, and that behavioural science theory can enhance engagement. Some fatigue-related conditions require “pacing”, where the person must balance the amount of activity they do with their disease symptoms, and not over-exert themselves. Overall, sustaining increases in activity in the long-term can be challenging, and people with disabilities and chronic health conditions are less likely to be physically active than people without such conditions, their health often suffers as a result.
What’s not clear, is how to reconcile this evidence with a weight-neutral, intuitive approach to movement. In my experience, it often feels like the “should” of exercise (particularly pertinent in disabilities and health conditions where specific exercises are the “treatment”) is in conflict with an intuitive or joyful movement approach, which advocates for moving in ways you enjoy. There are brilliant providers offering specialist programmes, either for disability (e.g. Chimera Health), or non-weight focussed practices (e.g. Tally Rye). I’d like to explore how we bring together intuitive movement practices, with “prescribed” movement for disabilities, and how we can use behavioural science to enhance engagement with it all more generally. We all know that sticking to something new is hard - hopefully this could help people to stick to the exercise they’re “supposed” to be doing, in a way that works for their bodies (which may fluctuate in ability day-to-day), and also to enjoy it.
The issue with weight loss is a much harder nut to crack. So much of health promotion (public health, healthcare, even wellness solutions) is centred on the idea that fat people should be working on intentional weight loss. However, we know from the evidence that this doesn’t work for most people in the long-term - people gain back the weight, and more. Paradigms such as “Health at Every Size” and intuitive eating aim to help people to improve their health, without considering (or trying to change) their weight - this feels hugely valuable in creating a world where people can feel good, without feeling ashamed of their bodies, or like they’re always “failing” when their weight inevitably rises again. In mainstream behavioural science, diet interventions in particular are often designed with the aim of delivering intentional weight loss as an outcome (although there has been some attention on the influence of weight stigma). As far as I have seen, the field hasn’t really adopted intuitive or weight-neutral approaches. This is despite the fact that behavioural science is really well-placed to focus on psychological and behavioural outcomes, rather than weight loss (given it's literally the science of behaviour!). The majority of research also tends to focus on conscious regulation of behaviours, and controlling impulses and urges rather than listening to them (as we might in intuitive eating or movement). What might behavioural science look like when applied to people’s health, in a weight-neutral and intuitive manner? What elements can we keep? What should we abandon? What are we missing?
I think the biggest challenge here will be finding the right motivators (or making the behaviours so easy that motivation is less important). Weight loss and appearance-related motivators are short-term, more immediate - this can give people the push they need to make changes. However, we also know that people don’t sustain these changes. So how do we get people to engage in changing and improving their health behaviour, in a long-term, sustainable way?
So what’s your plan, Rosie?
I want to explore this intersection between intuitive and weight-neutral approaches to health, diet and exercise for disability management, and behavioural science. I hope that this can:
- Help people like me to look after themselves a bit better, giving them an option which improves their health, while also accepting their bodies
- Help existing providers and experts in this space to enhance their (already amazing) work, by bringing in behavioural science principles, to enhance engagement and impact
- Champion a shift in the field of behavioural science away from “obesity” and towards a more weight-neutral, inclusive practice
There are a lot of existing experts in this space, for example nutritionists specialising in intuitive eating, or personal trainers specialising in specific health conditions. My intention isn’t to replace them, but to supercharge them. To bring these different fields together, to make them all better. With this in mind, I’ll be starting by looking at what existing evidence is there which relates to weight-neutral and disability-inclusive approaches to behaviour change (I already know of some, and I’m sure there’s more). I want to find all the possible resources and providers.
I don’t know yet what the end point of all this will be. I could discover that all of this already exists, and that my only role is in amplifying it. It could be that I create new frameworks, tools, or resources for applying behavioural science to weight-neutral and disability-inclusive practices. But most importantly, I just want to do what I can to help people to feel good and healthy in their bodies, regardless of their size or function.
But the first things I need to know are:
- What’s already out there? What am I missing here? Is this problem already solved, and I’m just not aware of it?
- What do you need? If you’ve got this far, this area clearly interests you* - so, what unanswered questions do you have? What are you really struggling with right now? Whether you’re a provider, a behavioural scientist, or you’re just working on your own health journey, I want to hear from you!
Complete this form here to tell me!
Ultimately, I don’t know where this journey will lead, but I’ll be sharing my learnings and progress here. Subscribe to make sure you don't miss a thing.
*or maybe you’re just being very supportive - if that’s you - hello and thank you 😘
